The Science Behind Player Injuries

Athletic injuries represent a complex intersection of biomechanics, physiology, psychology, and environmental factors. Understanding the scientific principles underlying these injuries is essential for developing effective prevention strategies and optimising recovery protocols.
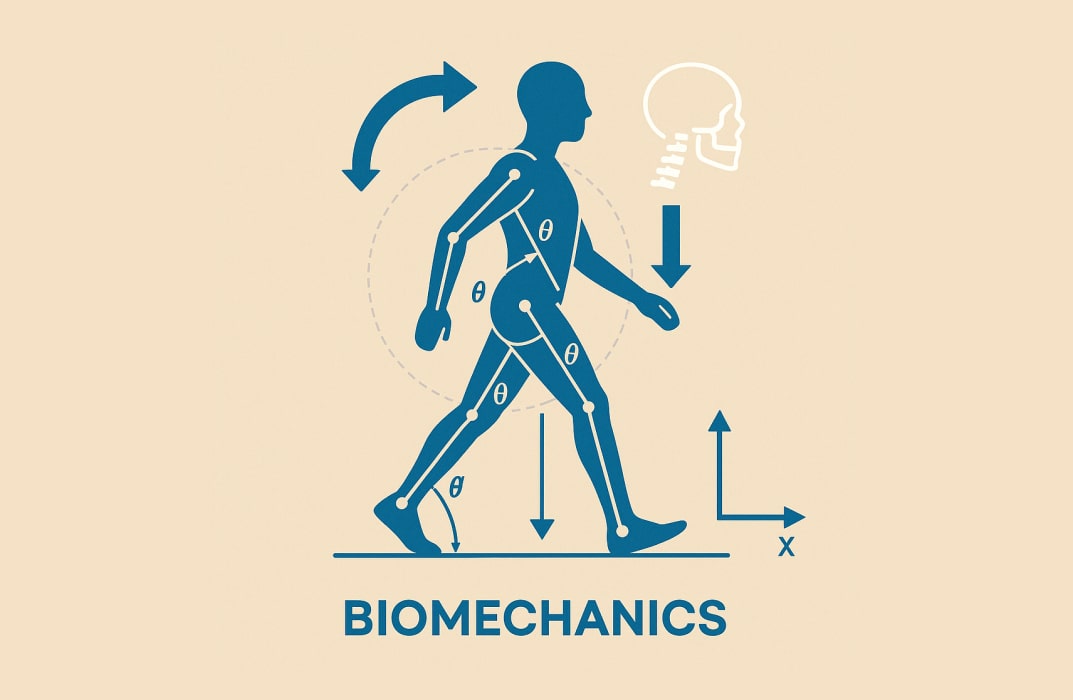
Biomechanical Foundations
The human body operates as an interconnected kinetic chain, where forces transfer through joints, muscles, tendons, and ligaments during athletic movement. Injuries often occur when these forces exceed the structural capacity of tissues.
During high-velocity movements like sprinting or cutting, ground reaction forces can exceed three to five times body weight, placing enormous stress on lower extremity structures.
When proper biomechanical alignment is compromised, whether through fatigue, poor technique, or muscular imbalances, these forces concentrate in vulnerable areas, increasing injury risk.
Anterior cruciate ligament (ACL) tears exemplify biomechanical failure. Research demonstrates that these injuries frequently occur during deceleration, landing, or pivoting movements when the knee experiences combined forces of rotation, valgus stress, and anterior tibial translation.
Female athletes exhibit a two- to eight-times higher ACL injury rate than males, partly due to biomechanical differences including greater knee valgus angles, reduced hamstring-to-quadriceps strength ratios, and hormonal influences on ligament laxity.
Tissue Mechanics and Failure Thresholds
Each biological tissue possesses distinct mechanical properties that determine injury susceptibility. Tendons, which connect muscle to bone, demonstrate viscoelastic behaviour—their stiffness and strength vary with loading rate. Sudden, explosive movements challenge tendons beyond their adaptive capacity, particularly when inadequate warm-up limits tissue pliability.
Chronic overload leads to tendinopathy, characterised by degenerative changes in collagen structure and increased proteoglycan content, which weakens the tissue and predisposes it to rupture.
Muscle strains typically occur at the musculotendinous junction, where contractile tissue transitions to collagen-rich tendon. High-speed eccentric contractions, where muscles lengthen under tension, generate the greatest forces and injury risk.
The hamstring muscle group, which crosses both hip and knee joints and functions eccentrically during the terminal swing phase of sprinting, represents the most commonly strained muscle in many sports.
Bone responds to mechanical stress through remodelling, a dynamic process balancing bone resorption and formation. When repetitive loading exceeds the bone's remodelling capacity, stress fractures develop.
These injuries follow a continuum from bone stress reaction to complete cortical fracture and commonly affect the tibia, metatarsals, and femoral neck in runners and jumping athletes.
Physiological Risk Factors
Fatigue fundamentally alters injury risk through multiple mechanisms. As muscles fatigue, they lose their ability to absorb shock effectively, transferring greater stress to passive structures like ligaments and cartilage.
Neuromuscular control deteriorates, compromising proprioception and increasing the likelihood of aberrant movement patterns. Studies consistently demonstrate higher injury rates during the latter stages of games and training sessions when fatigue accumulates.
Dehydration and electrolyte imbalances impair muscle function and increase cramping susceptibility.
Even modest fluid deficits of two per cent body weight can compromise cardiovascular function and thermoregulation, indirectly affecting performance and injury risk. Heat illness represents an extreme consequence of inadequate thermoregulation during intense exercise in hot environments.
Neurological and Sensorimotor Factors
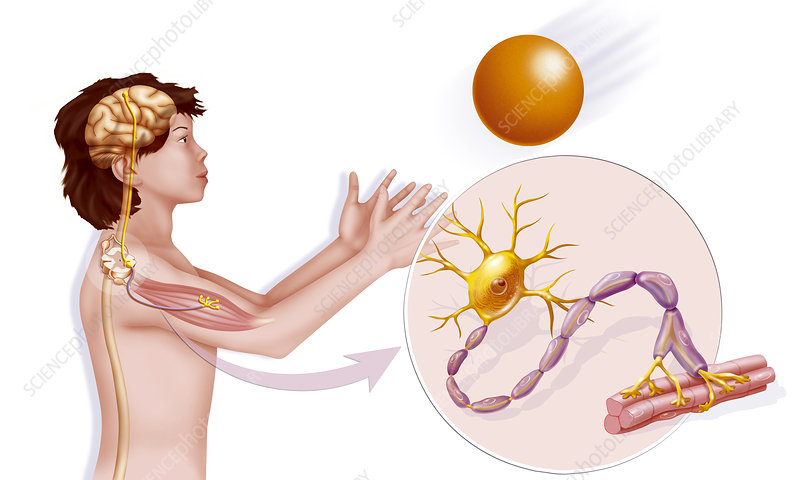
The neuromuscular system governs movement control through complex feedback loops involving proprioceptors, the central nervous system, and motor neurones.
READ MORE: Arsenal seal EFL Cup final spot with gritty win over Chelsea
Proprioception—the body's ability to sense joint position and movement—is critical for maintaining stability and executing coordinated movements.
Ankle sprains often damage mechanoreceptors in ligaments, compromising proprioceptive feedback and increasing the risk of recurrent injury if not properly rehabilitated.
Reaction time and anticipatory muscle activation patterns significantly influence injury risk. Athletes must activate stabilising muscles milliseconds before ground contact or impact.
Inadequate neuromuscular programming leaves joints vulnerable during these critical moments. Plyometric training and sport-specific drills enhance these protective mechanisms by improving the speed and coordination of muscle recruitment patterns.
Previous Injury and Scar Tissue
Prior injury stands as one of the strongest predictors of future injury. Scar tissue that forms during healing lacks the mechanical properties of native tissue—it's typically less elastic, has altered collagen fibre orientation, and possesses reduced tensile strength.
Incomplete rehabilitation compounds these structural deficiencies with persistent neuromuscular deficits, including strength asymmetries, reduced proprioception, and compensatory movement patterns that redistribute stress to other body regions.
Concussions illustrate the complexity of repeat injury risk. Following a concussion, the brain enters a period of metabolic vulnerability where cellular energy systems are compromised.
Sustaining another impact during this window, which may last days to weeks, can result in prolonged symptoms or, in rare cases, catastrophic outcomes like second impact syndrome.
Training Load and Recovery
The relationship between training load and injury risk follows a U-shaped curve. Insufficient training leaves athletes unprepared for competition demands, while excessive training without adequate recovery causes cumulative tissue damage and systemic fatigue.
The acute-to-chronic workload ratio comparing recent training volume to longer-term average load has emerged as a valuable metric for monitoring injury risk.
Rapid spikes in training intensity or volume, where acute load substantially exceeds chronic load, correlate strongly with increased injury incidence.
Recovery represents more than passive rest. During recovery periods, tissues repair microtrauma, glycogen stores replenish, inflammatory processes resolve, and the nervous system recuperates.
Sleep plays a particularly crucial role, with inadequate sleep duration and quality associated with significantly elevated injury rates. Athletes sleeping less than eight hours per night demonstrate up to 1.7 times greater injury risk than well-rested counterparts.
Environmental and Equipment Factors
Playing surfaces influence injury biomechanics. Natural grass provides more forgiveness than artificial turf, though modern synthetic surfaces have narrowed this gap.
Surface traction affects the forces transmitted through the body during cutting manoeuvres—excessive traction can increase non-contact ACL injury risk by preventing the foot from sliding, thereby concentrating rotational forces at the knee.
Footwear design impacts both performance and injury risk. Proper cushioning attenuates ground reaction forces, while appropriate support maintains alignment during dynamic movements.
However, excessive cushioning may diminish proprioceptive feedback, and overly restrictive shoes can alter natural foot mechanics.
Climate conditions affect tissue properties; cold temperatures reduce tissue compliance, increasing strain susceptibility, while hot, humid conditions elevate heat illness risk.
Psychological and Behavioural Dimensions
Psychological factors subtly but significantly influence injury vulnerability. High stress and anxiety elevate cortisol levels, which can impair tissue healing and immune function.
Attentional focus affects movement quality—distraction or excessive pressure can disrupt motor control. Athletes with certain personality traits, including high risk-taking tendencies or perfectionism coupled with reluctance to report symptoms, may engage in behaviours that increase injury exposure.
The psychological response to injury profoundly affects rehabilitation outcomes. Fear of re-injury can perpetuate compensatory movement patterns even after tissue healing completes.
Conversely, athletes who return to play prematurely, driven by competitive pressure or inadequate appreciation of injury severity, risk exacerbating initial damage or sustaining new injuries to compromised tissues.
Age and Developmental Considerations
Youth athletes face unique injury risks related to skeletal immaturity. Growth plates, areas of developing cartilage near bone ends, represent zones of weakness susceptible to injury.
Rapid growth during adolescence can temporarily reduce flexibility as bones lengthen faster than muscles and tendons adapt, creating imbalances that increase strain injury risk. Overuse injuries, including Osgood-Schlatter disease and Sever's disease, reflect repetitive stress on growing skeletal structures.
Ageing athletes contend with progressive tissue changes, including reduced collagen elasticity, decreased muscle mass and power, slower recovery rates, and diminished proprioception.
While these changes increase baseline injury risk, appropriate training modifications can substantially mitigate these effects. Master athletes often experience different injury patterns than youth, with a higher proportion of overuse injuries and degenerative conditions.
Integrative Injury Prevention
Modern injury prevention recognises that no single factor causes most injuries; rather, multiple risk factors interact dynamically.
The sequence of prevention model proposes that injuries result from complex interactions between internal risk factors (age, previous injury, anatomical alignment) and external risk factors (training load, equipment, environment), mediated by an inciting event.
Effective prevention requires comprehensive assessment addressing multiple domains—screening for biomechanical deficiencies, monitoring training loads, ensuring adequate recovery, optimising nutrition, and fostering psychological resilience.
Emerging technologies, including wearable sensors, motion capture systems, and artificial intelligence algorithms, offer unprecedented opportunities for personalised injury risk assessment.
These tools enable continuous monitoring of movement quality, training load, and physiological markers, potentially identifying elevated risk before injuries occur.
However, translating data into actionable interventions remains challenging and requires integration of technology with clinical expertise and individualised athlete management.
Understanding the multifaceted science behind player injuries empowers coaches, medical staff, and athletes to implement evidence-based strategies that reduce injury burden while optimising performance.
As research continues revealing the intricate mechanisms underlying athletic injuries, prevention and treatment approaches will become increasingly sophisticated and effective.


